WHAT DO PEOPLE WITH DIABETES ACTUALLY EAT?

Of all the people in the population, it is those with diabetes who have been exposed to the most dietary advice on how to eat to avoid the complications that often accompany the condition. In many ways, this guidance has been essentially the same as that given to the whole population on ways to eat a healthy diet. In the case of type 1 diabetes and people with type 2 diabetes that use insulin, there are additional instruction on the carbohydrate content of foods and how to space carbs according to insulin injections/infusions. In some diabetes clinics such as the Joslin (1) and Mayo Clinics (2) in the US, patients may be given information on the glycemic index of foods and how to swap high GI foods for low GI foods. The first clinic to do so was the International Diabetes Institute in Melbourne led by Professor Paul Zimmett in the 1990s (3) and the GI is now commonly used by people living with diabetes in Australia.
In the past, advice was fairly simple: people with diabetes were told to strictly avoid sugars because these were believed to be rapidly absorbed, causing spikes in blood glucose. While authorities now recognise that a small amount of sugar is fine, the rule has ‘stuck’ in the minds of many people, including the general population.
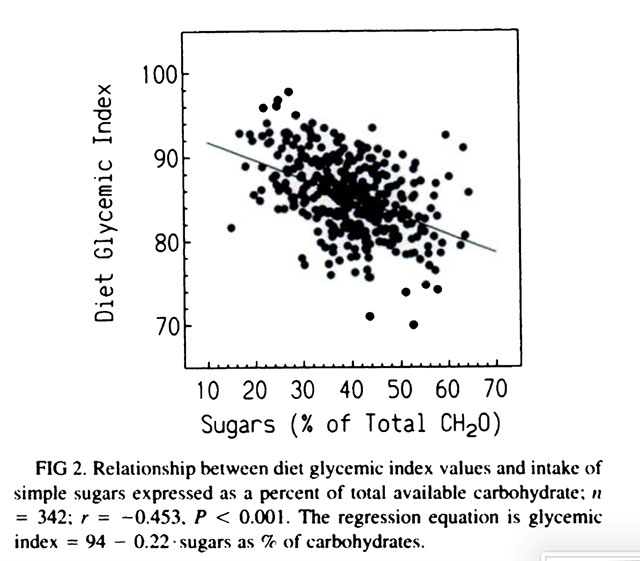
Do people with diabetes actually eat less sugar than the general population? In the 1990s, Professor Tom Wolever and his colleagues at the University of Toronto analysed the diet of 342 people with type 2 diabetes (4). Each had received dietary counselling from a dietitian with the aim of meeting the 1989 Canadian Diabetes Association dietary guidelines. Within 2 months of the advice, they recorded all food eaten over 3-days on 2 occasions (i.e., 6 days in total, the gold standard in dietetic research). I think it’s still the largest group that has ever been studied. On average, they ate 20% of their energy as protein (more than recommended), 33% as fat (again more than recommended at that time) and 40% as carbohydrate (less than recommended at that time). The mean GI was rather high: ~60 on the glucose = 100 scale, ranging from about 50 to 70. The most significant factor related to GI was the proportion of simple sugars (expressed as percent of total carbs). Interestingly, the higher the sugars intake, the lower the dietary GI, as shown in the Figure below. This might surprise most people, but the reason is clear: foods rich in sugars such as milk, yoghurt and fruits tend to have a lower GI than those of common starchy foods such as bread, rice, potatoes and breakfast cereals.
To be specific, starchy foods have GI values in the 70s, 80s and 90s, while sugary foods have GI values in the 40s, 50s and 60s. Many sugary foods contain fructose (or fruit sugar) which has a very low GI (=20) which is likely to be oxidised immediately. Only in extraordinarily high amounts does fructose lead to ill effects (5). Carbonated soft drinks (e.g., soda or pop), however, can have a higher GI because the bubbles increase the rate of stomach emptying and therefore absorption. Their GI is close to 70.
Fortunately, we can now find low GI versions of breads, rices, potatoes and breakfast cereals (6, 7). Being slowly digested and absorbed, they help you feel fuller for longer. They also stimulate less insulin and more GLP1, the same hormone that is the basis of drugs like Ozempic, Wegovy and Mounjaro.
In the 1980s, Professor Stephen Colagiuri and my husband Dr John Miller, conducted a crossover study in which volunteers with type 2 diabetes were randomly assigned to consume 45 g (11 teaspoons) of added sugar or an intense sweetener (aspartame) every day for 6 weeks (8). They then swapped over to the other sweetener for another 6 weeks. At study end, the addition of sucrose was found to have had no deleterious effect on glycemic control, lipids, glucose tolerance or insulin compared with Aspartame.
Finally, let’s return to the original question of what people with diabetes actually eat? Dr Alan Barclay, myself and colleagues measured the diet of Australians with diabetes as part of the Blue Mountains Eye study conducted in the 1990s (9). The diet of about 3600 older Australians (6% with diabetes) was assessed by a 145-item food frequency questionnaire. Those with diabetes (~160) were found to consume more protein and less sugars than the general population, but only 7 of them met all macronutrient recommendations and only 4 met the fibre target. Their average GI was 55, somewhat lower than that of the non-diabetes population.
Isn’t it strange that there is so little research on what people with diabetes eat, given the effort that goes into instruction? Perhaps studies have remained unpublished because the findings were not what researchers and clinicians wanted to see? Had all their efforts come to nought?
It’s extremely hard to change food habits and eating behaviour. So much is set by culture in childhood and even in utero. What is abundantly clear, however, is that a healthy diet comes in many flavours and colours, with different amounts of fat, protein and carbohydrate. The quality of these choices dictates how long you’ll live along with genetics and other environmental factors. My wish is that everyone can eat a healthy diet that they thoroughly enjoy with allowance for a small treat every day… and party foods at party time.
Read more:
- Joslin Education Team. Carbs, Protein and Fats – Their Effect on Glucose Levels. 2021.
- Mayo Clinic Staff. Low-glycemic index diet: What’s behind the claims? 2022.
- Baker Heart & Diabetes Institute. Carbohydrates and Glycaemic Index (GI). 2024.
- Wolever and colleagues. Determinants of diet glycemic index calculated retrospectively from diet records of 342 individuals with non-insulin-dependent diabetes mellitus. Am J Clin Nutr. 1994.
- Tappy and colleagues. Fructose-containing caloric sweeteners as a cause of obesity and metabolic disorders. J Exp Biol, 2018.
- www.glycemicindex.com
- www.gisymbol.com
- Colagiuri and colleagues. Metabolic effects of adding sucrose and aspartame to the diet of subjects with noninsulin-dependent diabetes mellitus. American Journal of Clinical Nutrition,1989.
- Barclay and colleagues. Macronutrient intake, glycaemic index and glycaemic load of older Australian subjects with and without diabetes: baseline data from the Blue Mountains Eye Study. British Journal of Nutrition, 2006.
Emeritus professor Jennie Brand-Miller held a Personal Chair in Human Nutrition in the Charles Perkins Centre and the School of Life and Environmental Sciences, at the University of Sydney until she retired in December 2022. She is recognised around the world for her work on carbohydrates and the glycemic index (or GI) of foods, with over 300 scientific publications. Her books about the glycemic index have been bestsellers and made the GI a household word.








