GI, SATURATED FAT AND YOUR LIVER
Do you know if you have a fatty liver? If that’s a yes, what can be done to treat it?
Thirty years ago, a vivacious redhead by the name of Dr Sandra Cabot wrote a wildly popular book called The Liver Cleansing Diet. I, like many others thought it was all a bit crazy. Mind you, we didn’t take the trouble to read her book but we were quick to criticise her on the basis that her diet didn’t have randomised controlled trials to back it up.
Fast forward to today and the state of one’s liver is known to be of prime importance to health, particular the degree of damage caused by alcohol, toxins, prescription and other drugs. Routinely, doctors will measure the levels of liver enzymes and proteins in the blood to assess the degree of damage.
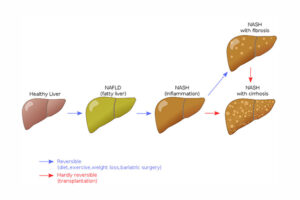
Three decades ago, we didn’t realise that fat accumulated in liver cells, not only in response to excessive alcohol, but also as a result of excess weight. We learned that some people developed a fatty liver more easily than others and often go on to develop inflammation of the liver (hepatitis) and even cirrhosis or hardening of the liver where scar tissue severely impacts its normal function, enough to cause severe pain and eventual death.
At first, General Medical Practitioners (GP) suspected that patients were not being entirely transparent about alcohol intake and were surprised to learn that it did not need to be present or excessive to develop the disease. The early stages of fatty liver without excessive alcohol intake went on to be known as non-alcoholic fatty liver disease (acronym NAFLD). In later stages of fatty liver disease, where there are signs of inflammation and liver cell damage, it is called non-alcoholic steatohepatitis (NASH). Prevalence of both conditions has soared as overweight and obesity increased rapidly around the world.
Today, fatty liver is suspected if liver enzyme levels are outside the normal range, blood triglyceride levels are high and HDL-cholesterol (good cholesterol) levels are low. The diagnosis can be confirmed by a MRI scan of the liver, but that’s usually not done routinely because of the expense.
So, if you have a fatty liver, what can you do about it? If you are overweight or obese, your GP will want you to lose some weight – as little as 5% (from say 100 kg to 95 kg) is often sufficient to improve all blood markers, including liver function tests.
If you are a regular reader of GI News, you’ll know that we recommend total meal replacements for a short period of time (4-12 weeks, depending on the degree of obesity) for safe and rapid weight loss. Studies like PREVIEW and DiRECT show how successful they are in not only producing substantial weight loss but also reversing chronic diseases such as type 2 diabetes, polycystic ovarian syndrome (PCOS) and hypertension (high blood pressure).
But weight loss is only part of the story. Optimising the balance of different foods, including fruits and vegetables, legumes, dairy, meat, seafood, poultry, nuts, seeds and healthy oils, while limiting the intake of ‘party foods’ (you know what I mean) to modest levels is the long term goal. The CSIRO’s Total WellBeing Diet online has been shown to be particularly effective in helping people lose weight safely using healthy foods and even daily treats.
Once your target weight loss has been achieved, maintaining the weight loss is critical to keeping the liver and other organs in the best shape possible. Which brings us to a recent well-designed study carried out by researchers Basset-Sagarminaga and colleagues at the University of Maastricht in the Netherlands.
Several studies have shown favourable effects of low-GI or low-saturated fat diets on liver fat content (known scientifically as intra-hepatic lipid, IHL), but these studies were performed under overfeeding conditions or extreme differences in GI or saturated fat to maximize the contrast between diets. However, by combining changes in GI AND saturated fat, we can mimic how people can improve their diet in a realistic setting. In the new study, the investigators studied the effect on liver fat content and substrate metabolism of both reducing GI and replacing saturated fat with polyunsaturated fat in typical amounts. They used the gold standard design – a randomized crossover study, in which 13 overweight participants were assigned randomly to one or other diet first and then the other. Thus, every participant consumed the two diets for two weeks each, one high in GI and saturated fat (high GI/SF) and one low in GI and saturated fat (low GI/SF) with identical macronutrient composition. The diets were equal in energy (kilojoule) content, consisted of habitual food items, and had a macronutrient composition that can be easily achieved in daily life (53% carbohydrate, 27% fats and 15% protein).
At the end of each diet period, liver fat content/composition and liver glycogen (carbohydrate) were measured by magnetic resonance spectroscopy. Additionally, fasted and postprandial (after-meal) liver fat synthesis and metabolic responses were assessed.
And the results? Liver fat was significantly lower (down by about 30%) after the two-week low-GI/SF diet than after the two-week high-GI/SF diet. Liver glycogen content, new lipid synthesis, fatty acid composition, and overnight substrate oxidation were similar between the two diets. However, glycemic responses to the low-GI/SF diet were reduced by the end of the two weeks, suggesting improvements in glucose tolerance.
This new study allows us to conclude that changes in macronutrient quality can have stunning effects (the authors call it drastic!) on liver fat and postprandial glycemia after just a brief intervention, even when total energy intake and the percentage of total fat and carbohydrate remain unchanged.
A healthy low GI diet is one simple short cut to a healthy diet. Choose pastas, legumes, lower GI potatoes and other starchy vegetables, and low GI brands of breads, rices, couscous, breakfast cereals and wholegrains. In selected parts of the world, you can make it easy by watching out for the certified GI Symbol on foods in your local supermarket.
Read more:
- Cabot. The Liver Cleansing Diet
- Raben and colleagues. The PREVIEW intervention study: Results from a 3-year randomized 2 x 2 factorial multinational trial investigating the role of protein, glycaemic index and physical activity for prevention of type 2 diabetes. Diabetes Obes Metab. 2021
- Lean and colleagues. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. 2018
- Basset-Sagarminaga and colleagues. Replacing Foods with a High-Glycemic Index and High in Saturated Fat by Alternatives with a Low Glycemic Index and Low Saturated Fat Reduces Hepatic Fat, Even in Isocaloric and Macronutrient Matched Conditions. Nutrients, 2023.
Emeritus professor Jennie Brand-Miller held a Personal Chair in Human Nutrition in the Charles Perkins Centre and the School of Life and Environmental Sciences, at the University of Sydney until she retired in December 2022. She is recognised around the world for her work on carbohydrates and the glycemic index (or GI) of foods, with over 300 scientific publications. Her books about the glycemic index have been bestsellers and made the GI a household word.








