INSULIN INDEX AND CARDIOVASCULAR RISK FACTORS IN PEOPLE WITH TYPE 2 DIABETES

Most people are probably not aware of the fact that many of the established risk factors for cardiovascular diseases (e.g., heart disease and stroke), like overweight/obesity (particularly abdominal), type 2 diabetes, high blood pressure and dyslipidaemia (high blood cholesterol and triglycerides), are associated with high blood insulin levels.
Furthermore, if you have three or more of these cardiovascular-disease risk factors, you have what is known as the metabolic syndrome, otherwise known as the insulin resistance syndrome, or simply “Syndrome X”. Unfortunately, the metabolic/insulin resistance syndrome is becoming increasingly common around the world, with approximately 1 in 3 people living with it in the USA and Australia, and 1 in 4 in the UK.
Insulin resistance occurs when the cells in our muscles, fat tissue, and liver don’t respond well to insulin and consequently can’t easily take up the sugar glucose from the blood. As a result, the pancreas makes more insulin to help glucose enter the cells.
It has long been known that consuming foods and drinks increases blood insulin levels – in particular, those high in available carbohydrate. However, the Insulin Index (II) was first conceived by researchers at the University of Sydney in 1997. It represents the effect of all foods and drinks on blood insulin levels, independent of their available carbohydrate content.
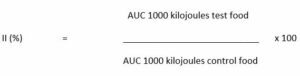
Using a method similar to that used to measure the glycemic index, 1000 kilojoules (240 Calories) worth of the control food (e.g., glucose) is consumed by participants and their blood insulin levels are measured over a 2 hour period. On a different day, participants consume a portion of food or drink (the test food) that also provides 1000 kilojoules, and blood insulin levels are measured again over a 2 hour period. The area under the blood insulin curve (AUC) is calculated for both the control and test foods, and the results are used to calculate the II according to the following formula:
Also, like the GI and glycemic load (GL), the dietary insulin index (DII) and the dietary insulin load (DIL) are computed based on the II values of foods and drinks that comprise a person’s diet. Lower DII and DIL values indicate lower insulin responses to foods, meals or diets.
A recently published study by Dr Javad Anjom-Shoae and colleagues investigated the association between DII and DIL and risk of developing the metabolic/insulin resistance syndrome in 826 overweight, middle-aged people living with type 2 diabetes.
People with higher DII and DIL values were shown to have increased odds of developing the metabolic/insulin resistance syndrome – a 30% and 98% increase in risk for DII and DIL, respectively. With respect to abdominal obesity, there was a 106% and 190% increase in risk for people with high DII and DIL, respectively. There was also a significant association between having a high DIL and general obesity (101% increase in risk), but not DII. Dyslipidaemia and high blood pressure were not associated with DII or DIL, however.
This observational study provides further evidence that the insulin index may be something to consider when choosing foods and beverages, and designing meals and diets. However, more research is needed to confirm these associations, and also we need to measure the II of more foods and drinks to make the tool practicable.
Read more:
-
US National Heart, Lung, and Blood Institute. What Is Metabolic Syndrome?
-
Holt and colleagues. An insulin index of foods: the insulin demand generated by 1000-kJ portions of common foods, AJCN, 1997.
-
Anjom-Shoae and colleagues. Dietary insulin index and load in relation to cardiometabolic risk factors in patients with type 2 diabetes mellitus: A cross-sectional study on the RaNCD cohort study. Nutrition. 2022.








